Depression and insomnia often coexist, creating a complex and challenging scenario for both patients and healthcare providers. The intertwining nature of these conditions can exacerbate symptoms and hinder treatment progress. In such cases, finding the most effective medications becomes paramount. This article delves into the realm of pharmacotherapy, exploring the best medications for managing depression and insomnia simultaneously.
Understanding Depression and Insomnia: Before delving into medication options, it’s crucial to grasp the intricacies of depression and insomnia individually and their interconnectedness. Depression is a mood disorder characterized by persistent feelings of sadness, hopelessness, and disinterest in previously enjoyed activities. Insomnia, on the other hand, involves difficulty falling or staying asleep, leading to poor sleep quality and daytime impairment. Research indicates a bidirectional relationship between these conditions, with insomnia increasing the risk of developing depression and vice versa.
The Need for Dual Treatment: Addressing depression and insomnia simultaneously is essential for comprehensive management. Treating one condition while neglecting the other can result in incomplete symptom relief and potential relapse. Moreover, untreated insomnia can undermine the efficacy of antidepressant medications, leading to treatment resistance. Therefore, a holistic approach that targets both depression and insomnia is paramount for optimal outcomes.
Medication Options:
Antidepressants:
Selective Serotonin Reuptake Inhibitors (SSRIs): SSRIs, such as sertraline, fluoxetine, and escitalopram, are commonly prescribed as first-line treatments for depression. These medications work by increasing the levels of serotonin, a neurotransmitter implicated in mood regulation. While SSRIs may improve depressive symptoms, their impact on insomnia varies among individuals.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): SNRIs like venlafaxine and duloxetine also target serotonin levels while additionally affecting norepinephrine levels. They may offer benefits for both depression and insomnia, although individual responses can vary.
Tricyclic Antidepressants (TCAs): TCAs, such as amitriptyline and nortriptyline, are older antidepressants with potent sedative properties. While effective in managing depression and promoting sleep, they carry a higher risk of side effects compared to newer agents.
Atypical Antidepressants: Medications like mirtazapine and trazodone possess sedative properties and are often prescribed off-label to address both depression and insomnia. Mirtazapine, in particular, is known for its sleep-enhancing effects due to its histamine-blocking properties.
Sedative-Hypnotics:
Benzodiazepines: Benzodiazepines, including diazepam and lorazepam, are central nervous system depressants commonly used to induce sleep. However, their long-term use is associated with tolerance, dependence, and withdrawal symptoms, making them less suitable for chronic insomnia management.
Non-Benzodiazepine Hypnotics: Zolpidem, zaleplon, and eszopiclone belong to this class of medications, which offer similar sedative effects to benzodiazepines but with a lower risk of dependence. They are typically prescribed for short-term insomnia treatment.
Melatonin Receptor Agonists: Ramelteon and tasimelteon target melatonin receptors, regulating the sleep-wake cycle. These medications are particularly beneficial for individuals with circadian rhythm disturbances, such as delayed sleep phase disorder.
Combination Therapies:
Combining antidepressants with sedative-hypnotics or other adjunctive agents is a common strategy for managing comorbid depression and insomnia. However, caution must be exercised to minimize the risk of drug interactions, additive side effects, and polypharmacy-related complications.
For instance, combining an SSRI or SNRI with a low-dose sedative-hypnotic or mirtazapine may synergistically alleviate depressive symptoms while addressing sleep disturbances.
Individualized Treatment Approach:
Choosing the best medication(s) for depression and insomnia requires a personalized approach that considers various factors, including:
Symptom severity and duration
Comorbid medical and psychiatric conditions
Medication tolerability and side effect profile
Patient preferences and treatment goals
Potential drug interactions and contraindications
Previous treatment response
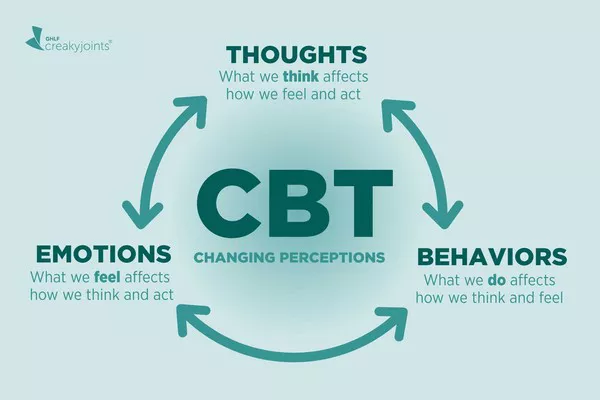
Healthcare providers should engage in thorough clinical assessments and ongoing monitoring to tailor treatment regimens accordingly. Additionally, non-pharmacological interventions such as cognitive-behavioral therapy for insomnia (CBT-I), lifestyle modifications, and stress management techniques complement pharmacotherapy and enhance overall treatment outcomes.
Conclusion:
Managing depression and insomnia concurrently presents a clinical challenge necessitating a multifaceted approach. While pharmacotherapy plays a central role, it should be integrated with non-pharmacological interventions for comprehensive care. By understanding the mechanisms of action, side effect profiles, and individual patient factors, healthcare providers can optimize treatment strategies and improve the quality of life for individuals grappling with these debilitating conditions.
FAQs
Which antidepressant is best for insomnia?
Mirtazapine, an atypical antidepressant, is often preferred for individuals with insomnia. Its sedating effect can improve sleep quality, making it beneficial for those experiencing both depression and sleep disturbances. Mirtazapine targets different neurotransmitters than typical SSRIs, potentially mitigating insomnia symptoms.
What medicine helps with sleep and depression?
Trazodone is frequently prescribed to address both depression and sleep issues. It acts as a serotonin antagonist and reuptake inhibitor, alleviating depressive symptoms, while its sedating properties aid in improving sleep quality. Trazodone is particularly useful for individuals experiencing insomnia alongside depression.
What antidepressant is least likely to cause insomnia?
Among antidepressants, tricyclic antidepressants (TCAs) such as amitriptyline and doxepin are less likely to cause insomnia compared to SSRIs or SNRIs. TCAs tend to have stronger sedative effects, which can aid in promoting sleep and may be beneficial for individuals prone to insomnia as a side effect of antidepressant treatment.
Related topics:
- A Glimpse into the Inpatient Experience for Depression
- Unlocking Hope: Finding the Best Antidepressant for Stroke Patients
- Major Depression: Can It Be Cured?